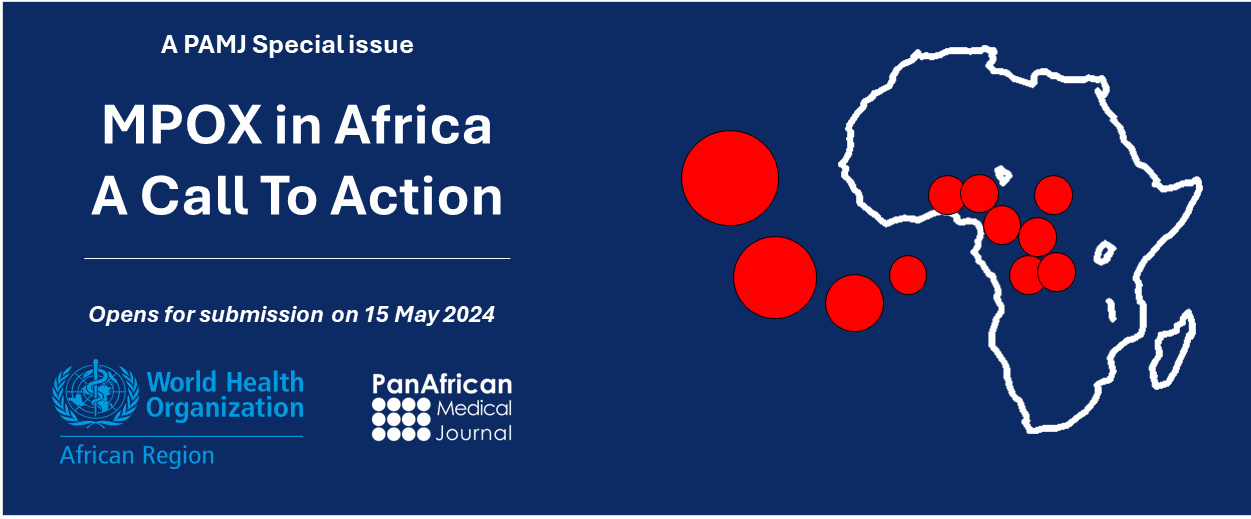
PAMJ Call for papers: The Surge of Mpox in African Countries - A Global Call to Action (Special Issue)
24 Apr 2024 / Announcement
About this special issue
 MPOX, formerly known as Monkeypox, is a zoonotic disease caused by the Monkeypox virus, belonging to the Orthopoxvirus genus within the Poxviridae family. Although the virus first human case of mpox was identified in the Democratic Republic of Congo (DRC, formerly Zaire) as far back as 1970, it remained under relative neglect by the global community until the first global outbreak in 2022. This prompted the World Health Organization to declare mpox a Public Health Emergency of International Concern (PHEIC) in July 2022. As of 22 December 2023, close to 93,000 laboratory-confirmed mpox cases and 171 deaths have been reported from 116 countries, including 2,126 cases and 22 deaths from endemic regions of Africa.
MPOX, formerly known as Monkeypox, is a zoonotic disease caused by the Monkeypox virus, belonging to the Orthopoxvirus genus within the Poxviridae family. Although the virus first human case of mpox was identified in the Democratic Republic of Congo (DRC, formerly Zaire) as far back as 1970, it remained under relative neglect by the global community until the first global outbreak in 2022. This prompted the World Health Organization to declare mpox a Public Health Emergency of International Concern (PHEIC) in July 2022. As of 22 December 2023, close to 93,000 laboratory-confirmed mpox cases and 171 deaths have been reported from 116 countries, including 2,126 cases and 22 deaths from endemic regions of Africa.
While outbreaks outside of Africa were swiftly controlled, the situation in Africa, particularly in the DRC, continues to raise concerns. From 1st Jan 2022 to November 2023, DRC reported 19,034 suspected cases and 820 deaths, of which 13,357 cases and 607 deaths were reported from January to December 2023 alone. Of particular concern is the significant feature of sexual transmission in the DRC, indicating a pressing need for comprehensive in-country and regional response efforts.
The ongoing DRC outbreak and concerns for regional mpox containment in endemic African countries prompted the organization of an emergency regional meeting by the WHO, Africa CDC, Institut National de Recherche Biomédicale (INRB), and UNICEF. The meeting was held in Kinshasa DRC from April 11th to 13th, 2024, and convened stakeholders from endemic and at-risk countries, multilateral and bilateral partners, funding agencies, and research institutions to assess the current outbreak and devise a regional response strategy. Among its outcomes, the meeting formulated a strategic approach to address significant knowledge gaps essential for informing effective mpox response efforts.
Peer-reviewed literature on mpox in Africa, particularly articles published in African journals, remains scarce. To address this gap, PAMJ, in partnership with the WHO AFRO Health Emergency programs supports this supplement, which aims to contribute to the body of knowledge on mpox in endemic African countries.
In this special issue, supported by the WHO AFRO Health Emergencies Programme (WHE), the Pan African Medical Journal (PAMJ) welcomes submissions related to all aspects of mpox in Africa, including epidemiology, research, clinical practice, outbreak investigation and response, and other relevant mpox data and activities in Africa. Submissions focusing on mpox research conducted outside Africa will be considered if deemed relevant to outbreak response efforts in endemic African countries. Except editorials, all submissions will undergo external peer review.
- Supported by: WHO AFRO Health Emergencies Programme
- Submission languages: English and French.
- Cost to authors: none.
Timelines
- Submissions open: 15 May 2024
- Submissions close: 30 November 2025
- Online publication: on a rolling basis, from 10 January to December 2025.
The supplement will focus on the following thematic areas:
- Epidemiology and genomics: Exploring disease burden, transmission patterns and genomics, and associated risks of mpox, with particular emphasis on its impact among children, underserved communities (e.g., remote, poor, and rural areas), and populations at high risk of, or affected by sexual transmission, as well as health care workers and pregnant women.
- Clinical features and treatments: Examining the clinical manifestations of mpox, treatment options available in Africa, treatment outcomes, and any existing co-morbidities associated with the disease.
- Social determinants and gender dynamics: Investigating the influence of social determinants on mpox transmission and outcomes, while also examining gender dynamics that may affect vulnerability or access to care.
- Community engagement: Assessing strategies for effectively engaging communities in mpox prevention, detection, and response efforts, including community-based interventions and participatory approaches.
- Implementation science and policy: Data reports on, or contributions for approach to translating mpox evidence into policy and practice and analysing the formulation and implementation of policies aimed at mpox prevention, control, and management, including considerations for policy alignment with broader health and development agendas.
Authors are invited to submit in the following categories:
|
|
Check the PAMJ Journal Instructions for Authors.
Guest Editors
 |
Jean B. Nachega, MD, MPH, PhD, DTM&H, FAAS (Stellenbosch University, South Africa and University of Pittsburgh School of Public Health, PA, USA). Pr. Jean Nachega is a physician who is an Associate Professor of Medicine at the University of Pittsburgh. He is an infectious diseases doctor with a focus on improving the public health outcomes of people infected with HIV/AIDS. He is a Fellow of the African Academy of Sciences. |
|
|
|
 |
Nadia A. Sam-Agudu, MD, CTropMed (Institute of Human Virology Nigeria, University of Cape Coast School of Medical Sciences, Ghana, and University of Minnesota Medical School). Dr. Nadia is a clinician-scientist and Professor of Pediatrics in Infectious Diseases at the University of Minnesota USA, the Senior Technical Advisor for Pediatric and Adolescent HIV at the Institute of Human Virology Nigeria, and a faculty of the University of Cape Coast, Ghana. Her research focuses on major infectious diseases affecting children in African countries, including HIV, tuberculosis, COVID-19 and mpox. Dr. Sam-Agudu also applies her implementation science expertise to the delivery of infectious disease prevention and treatment interventions. She leads the Central and West Africa Implementation Science Alliance (CAWISA). |
|
|
|
 |
Boghuma K. Titanji, MD, MSc, PhD, DTM&H (Emory University School of Medicine, Altanta, GA, USA). Dr. Titanji is currently an assistant professor of medicine and has 4 parallel career interests: translational and clinical HIV research, science communication, emerging infectious diseases, and global health advocacy. Her clinical focus is people with HIV, and her current research focuses on chronic inflammation as a mediator of cardiovascular disease in people with HIV. In addition, she is passionate about leveraging translational research to improve the care of people with HIV, global health equity and using science to influence health policy through science communication and advocacy. |
|
|
|
 |
Dr Fiona Braka, MD, MPH (Emergency Response Manager, WHO Regional Office for Africa, Brazzaville, Congo Republic) Dr Fiona Braka is the Emergency Response Manager of the World Health Organization Regional Office for Africa based in Brazzaville, Congo. She leads the regional response operations to acute and protracted health emergencies including disease outbreaks and humanitarian crises. Her role also entails coordination of AFRO support to countries to strengthen their local capacities for emergency response through the EPR SURGE initiative. Dr Braka has two decades of national and international experience with the World Health Organization. Before joining the regional office in 2021, she served in different capacities in Nigeria, Ethiopia and Uganda where she led WHO efforts to eradicate wild polio virus and supported the national governments to strengthen their vaccination programmes. |
|
|
|
 |
Placide Mbala-Kingenbeni, MD, PhD (Institut National de Recherche Biomédicale and University of Kinshasa, Democratic Republic of the Congo. Dr Placide Mbala-Kingebeni is a Medical Doctor and virologist, he has participated in several research studies and in the control of several epidemics caused by zoonotic diseases such as Ebola and monkeypox, under the supervision of Professor Muyembe. He is currently Head of the Epidemiology and Global Health Department, and Head of the Pathogen Genomics Laboratory at the INRB. |
 |
Joseph Chukwudi Okeibunor,MSc, PhD (WHO Regional Office for Africa, Brazzaville, Congo Republic) Joseph Chukwudi Okeibunor leads the research activities in the Emergency Preparedness (EMP) unit of the Emergency Preparedness and Response (EPR) program in the WHO AFRO. He coordinated research in various capacities in WHO/AFRO, first, as Immunization Social Scientist for Immunization and Polio Eradication programmes; then as Lead Research & Development, including Digital Health in the Assistant Regional Directors cluster of WHO AFRO. In these capacities he coordinated the publication of several special issues of different journal on different disease pathogens in WHO/AFRO, thereby documenting various best practices WHO AFRO engaged in combatting health challenges, especially disease outbreaks in the region. Before joining WHO in 2012, he was Professor of Sociology/Anthropology in the University of Nigeria, Nsukka, and Fellow in International Health from Harvard School of Public Health, Harvard University, Boston Massachusetts, USA. |

Pan African Medical Journal
This article is published by the editorial office of the PAMJ (KENYA)
